- Transthoracic ECHO (TTE)
- Transesophageal Echocardiogram (TEE)
- Echocardiography / Stress Echocardiogram
- Nuclear Cardiology
- Cardiac Stress Testing
- Positron Emission Tomography (PET) scan
- Electrocardiogram (EKG)
- Holter Monitoring
- Peripheral Vascular Studies
Transthoracic ECHO (TTE)
How the Test is Performed
TTE is the type of echocardiogram that most people will have. Also called an Echo, it is a type of ultrasound that uses high-pitched sound waves that are sent through a device called a transducer. The device picks up echoes of the sound waves as they bounce off the different parts of your heart.
- One of our trained/registered sonographers will perform the test and then one of our cardiologists will interpret the results.
- A transducer, which is an instrument that converts variations in a physical quantity, such as pressure or brightness, into an electrical signal, or vice versa, is placed on the ribs near the breastbone and directed toward the heart. The device will then release high-frequency sound waves to take an image. Other images will be taken in other locations of the body as well, including underneath and slightly to the left of the breast and in the upper abdomen.
- The transducer will pick up echoing sound waves and then transmit them as electrical impulses. The Echocardiography machine converts these impulses into moving pictures of the heart. Still pictures are taken also.
- A Doppler Echocardiogram records the motion of blood through the heart.
An Echocardiogram enables the doctor to see the heart beating, the heart valves and other structures moving.
In some cases, lungs, ribs, or body tissue may prevent sound waves and echoes from providing a clear picture of the heart functioning. The Sonographer may inject a small amount of liquid (contrast) through intravenous medication administration (IV) to get a better look at the inside of the heart.
Rarely, more invasive testing using special echocardiography probes are needed.
How to Prepare for the Test
No special steps are needed before a regular echo (TTE) test. If you are having a transeosphageal echo (TEE), you will not be able to eat or drink after midnight the night before or 6-8 hours before the test.
How the Test will Feel
- You will need to take off your clothes, from the waist up, and lay down on an exam table on your back.
- Electrodes will be placed on your chest to monitor your heart beat.
- A gel is spread over your chest and the transducer will be moved over your skin. You will feel a slight pressure on your chest from the transducer.
- You may be asked to breathe-in a specific way or to roll over onto your left side. Sometimes a special bed is used to help you stay in the proper position.
Why the Test is Performed
This test is done to evaluate the valves and chambers of the heart from the outside of your body. The echocardiogram can help detect:
- Abnormal heart valves
- Abnormal heart rhythms
- Congenital heart disease
- Damage to the heart muscle from a heart attack
- Heart murmurs
- Inflammation (pericarditis) or fluid in the sac around the heart (pericardial effusion)
- Infection on or around the heart valves (infectious endocarditis)
- Pulmonary hypertension
- Ability of the heart to pump (for people with heart failure)
- Source of a blood clot after a stroke or TIA
Your healthcare provider may recommend a transesophageal echocardiogram (TEE) if:
- The regular or transthoracic echocardiogram is unclear. Unclear results may be due to the shape of your chest, lung disease, or excess body fat.
- An area of the heart needs to be looked at in more detail.
Normal Results
A normal echocardiogram reveals normal heart valves and chambers with normal heart wall movement.
What Abnormal Results May Indicate
An abnormal echocardiogram can mean many things. Some abnormalities are very minor and do not pose major risks. Other abnormalities are signs of serious heart disease. In this case, you will need more tests to be performed by your specialist. It is very important to talk about the results of your echocardiogram with your healthcare provider.
Risks
There are no known risks from an external transthoracic echocardiogram (TTE) test.
Considerations
Abnormal results may indicate:
- Heart valve disease
- Cardiomyopathy
- Pericardial effusion
- Other heart abnormalities
This test is used to evaluate and monitor many different heart conditions.
Transesophageal Echocardiogram (TEE)
Transesophageal echo (TEE) is used when your doctor needs a more detailed view of your heart. For example, TEE may be used to look for blood clots in your heart. A doctor, not a sonographer, performs this type of echo.
The test uses the same technology as transthoracic echo, but the transducer is attached to the end of a flexible tube. The tube will be guided down your throat and into your esophagus (the passage leading from your mouth to your stomach). From this angle, your doctor can get a more detailed image of the heart and major blood vessels leading to and from the heart.
For TEE, you’ll likely be given medicine to help you relax during the test. The medicine will be injected into one of your veins. Your blood pressure, the oxygen content of your blood, and other vital signs will be checked during the test. You’ll be given oxygen through a tube in your nose. If you wear dentures or partials, you’ll have to remove them.
The back of your mouth will be numbed with a gel or a spray so that you don’t gag when the transducer is put down your throat. The tube with the transducer on the end will be gently placed in your throat and guided down until it’s in place behind the heart.
The pictures of your heart are then recorded as your doctor moves the transducer around in your esophagus and stomach. You shouldn’t feel any discomfort as this happens.
Although the imaging usually takes less than an hour, you may be watched for a few hours at the doctor’s office or hospital after the test.
Echocardiography / Stress Echocardiogram
Stress echocardiography is a test that uses ultrasound imaging to determine how the heart muscles respond to stress. It is mainly used to diagnose and evaluate coronary artery disease.
How the Test is Performed
A stress echocardiogram includes the following steps:
A resting echocardiogram will be done first.
- You will exercise or be given medicine until you reach the target heart rate. This helps reveal how your heart works when you are active.
- Your blood pressure and heart rhythm (ECG) will be monitored throughout the procedure.
- Ultrasound images will be recorded during the procedure.
- Another echocardiogram is taken immediately after your target heart rate has been reached.
- The ultrasound images will reveal any parts of the heart that may not be receiving enough blood or oxygen because of blocked arteries.
This test differs from an exercise stress test, which does not use ultrasound images.
How to Prepare for the Test
Ask your healthcare provider if you should take any of your routine medicines on the day of the test (especially if you are taking heart medication). Some medicines may interfere with test results.
DO NOT eat or drink for at least 3 hours before the test. Wear loose, comfortable clothing.
How the Test Will Feel
Electrodes (conductive patches) will be placed on your chest, arms, and legs to record the heart’s activity. The preparation of the electrode sites on your chest may produce a mild burning or stinging sensation.
The blood pressure cuff on your arm will be inflated every few minutes, producing a squeezing sensation that may feel tight. Baseline measurements of heart rate and blood pressure will be taken before you start exercising.
You will start walking on a treadmill or pedaling a stationary bicycle. The pace and incline of the treadmill will gradually be increased.
If you are not able to exercise, you will receive a medication such as dobutamine or persantine through a vein (intravenous line). This type of medicine is given to increase your heart rate to a certain level. You may feel your heart beating more rapidly and forcefully. This is called a pharmacologic stress test.
Rarely, people experience chest discomfort, palpitations, dizziness, or shortness of breath during the test.
Why the Test is Performed
The test is performed to see whether your heart muscle is getting enough blood flow and, therefore, enough oxygen when it is working hard (under stress). The purpose is to discover and potentially treat any blockage or disease before serious or life-threatening problems develop.
Your doctor may request this test if you:
- Have new symptoms of angina or chest pain
- Have angina that is becoming worse
- Have recently had a heart attack
- Are at high risk for heart disease (before having surgery or when beginning an exercise program)
- Have heart valve problems
Risks
The risks are very low, and healthcare professionals will monitor you during the entire procedure. Rare complications include:
- Abnormal heart rhythm
- Collapse
- Heart attack
Considerations
A stress echocardiogram is a very effective, noninvasive test that can help determine whether you have blockages in your coronary arteries. If there are blockages, it can determine the severity of the problem. Early diagnosis and monitoring of heart disease allows treatment to begin early. This test does not require any radiation.
Nuclear Cardiology
Nuclear Cardiology
We offer noninvasive tests, both SPECT and PET scans to evaluate heart disease using a small amount of radioactive substance. It is injected into a vein and its presence is detected by a nuclear medicine imaging camera. Images reveal areas of the heart that are not getting enough blood.
These tests are called myocardial perfusion imaging. Your cardiologist will determine which test is most appropriate for you.
Myocardial Perfusion Imaging (SPECT & PET)
Myocardial perfusion images are combined with exercise to assess the blood flow to the heart muscle. Exercise is usually in the form of walking on a treadmill. A “chemical” stress test using the drug regadenosine/lexiscan may be performed in patients who are not able to exercise maximally, providing similar information about the heart’s blood flow without walking on a treadmill.
Myocardial perfusion studies can thus identify areas of the heart muscle that have an inadequate blood supply as well as the areas of heart muscle that are scarred from a heart attack. In addition to the localization of the coronary artery with atherosclerosis, myocardial perfusion studies quantify the extent of the heart muscle with a limited blood flow and can also provide information about the pumping function of the heart. Thus, it is superior to routine exercise stress testing and provides the necessary information to help identify which patients are at an increased risk for a heart attack and may be candidates for invasive procedures such as coronary angiography, angioplasty and heart surgery.
How the Test is Performed (Cardiac SPECT)
A small amount of an imaging agent – thallium or sestamibi (Cardiolite) or tetrofosmin (Myoview), is injected into the bloodstream during rest and during exercise or chemical stress. A scanning device (SPECT camera) is used to measure the uptake by the heart of the imaging material. If there is significant blockage of a coronary artery, the heart muscle may not get enough of a blood supply in the setting of exercise or during chemical stress. This decrease in blood flow will be detected by the images.
Then, you will lie on a narrow table that slides into a circular-shaped scanner. You must lie still during test. Too much movement can blur images and cause errors.
Positron Emission Tomography (Cardiac PET)
Cardiac PET is an imaging technique that produces a superior image of the heart in patients who require it. A PET scan is noninvasive and is used to provide information about both the blood supply to the heart muscle and the metabolic activity of the heart. PET studies can outline the heart muscle that is not getting adequate blood flow because of the blockage in the arteries of the heart. These studies can also show the heart muscle that has been scarred from past heart attacks, and also what has been damaged but has the potential to recover if a bypass surgery or an angioplasty is performed on the patient. This ability to distinguish irreversibly damaged heart muscle from damaged heart muscle with a potential to recover its function after bypass surgery or angioplasty is a major strength of PET imaging. These studies can also help in making determinations about candidacy for bypass surgery or angioplasty. With the wider availability of PET imaging cameras, the use of PET imaging has increased significantly in the last few years.
How the Test is Performed (Cardiac PET)
A PET scan uses a radioactive material (tracer). The tracer is given through a vein (IV), most often on the inside of your elbow. The tracer travels through your blood and collects in the heart. This helps the cardiologist see certain areas of concern more clearly.
Then, you will lie on a narrow table that slides into a circular-shaped scanner. The PET detects signals from the tracer. A computer changes the signals into digital color pictures. The images are displayed on a monitor for your doctor to read.
You must lie still during test. Too much movement can blur images and cause errors.
How to Prepare for the Tests
You may be asked not to eat anything for 4 – 6 hours before the scan. You will be able to drink water.
Tell your healthcare provider if:
- You are pregnant or think you might be pregnant.
- Always tell your healthcare provider about the medicines you are taking, including those bought without a prescription. Sometimes, medications may interfere with the test results.
How the Tests will Feel
You may feel a sharp sting when the needle with the tracer is placed into your vein.
SPECT or PET scans cause no pain. The table may be hard or cold, but you can request a blanket or pillow.
A trained certified nuclear medicine technician will be in attendance and available for assistance at all times.
There is little or no recovery time and most patients are able to exit test without delay.
Risks
The amount of radiation used in SPECT and PET scans are safe and strictly low diagnostic levels. SPECT tracers are relatively short lived and patients are advised to drink amble fluids to expedite clearance of tracers from their bodies. PET tracers exit the body within 2-10 hours.
Tell your doctor before having these tests if you are pregnant or breast feeding.
Rarely, people may have an allergic reaction to the tracer material. Some people have pain, redness, or swelling at the injection site.
Cardiac Stress Testing
A stress test is a medical examination performed to evaluate arterial blood flow to the myocardium (heart muscle) during physical exercise, compared to blood flow while at rest. As an exercise test, the results can also reflect overall physical fitness. These tests do not assess emotional stress or other connotations of the term.
You will walk on a treadmill while the electrical activity of your heart is measured with an electrocardiogram (ECG), and blood pressure readings are taken. This will measure your heart’s reaction to your body’s increased need for oxygen.
The test continues until you reach a target heart rate, unless complications such as chest pain or an exaggerated rise in blood pressure develop. You will continue to be monitored for 10 – 15 minutes after exercising, or until your heart rate returns to baseline.
How to Prepare for the Test
You must not eat, smoke, or drink beverages containing caffeine or alcohol for 3 hours before the test. You should continue all medications unless instructed otherwise.
Wear comfortable shoes and loose clothing to allow for exercise.
Tell your doctor if you are taking sildenafil citrate (Viagra) and have taken a dose within the past 24 hours. This is necessary because nitroglycerin, which is sometimes given during a stress test to relieve chest pain, should not be given to a person who has recently taken Viagra, since the combination can cause a serious drop in blood pressure.
How the Test Will Feel
Electrodes (conductive patches) will be placed on your chest, arms, and legs to record the heart’s activity.
The blood pressure cuff on your arm will be inflated every few minutes, producing a squeezing sensation that may feel tight. Baseline measurements of heart rate and blood pressure will be taken before exercise starts.
You will start walking on a treadmill. The pace and incline of the treadmill will gradually be increased.
Rarely, people experience chest discomfort, palpitations, dizziness, or shortness of breath during the test.
Why the Test is Performed
A stress test is performed to determine causes of chest pain, the exercise capacity of the heart, appropriate exercise levels in those beginning an exercise program, and to identify rhythm disturbances during exercise. There may be additional reasons that your health care provider requests this test.
Normal Results
Normally, heart rate increases in proportion to the workload and attains endurance levels appropriate for age and conditioning level.
What Abnormal Results Mean
Abnormal results may indicate arrhythmias during exercise, stress on the heart provoked by exercise, possible coronary artery disease (blockage in the arteries), or lack of aerobic fitness.
Risks
Stress tests are generally safe. Some patients may have chest pain or may faint or collapse. A heart attack or dangerous irregular rhythm rarely occurs. Persons who are likely to have such complications are usually already known to have weak hearts, so they are not given this test.
Positron Emission Tomography (PET) Scan
A positron emission tomography (PET) scan is an imaging test that uses a radioactive substance called a tracer to look for disease in the body.
A PET scan shows how organs and tissues are working. This is different than magnetic resonance imaging (MRI) and computed tomography (CT), which show the structure of and blood flow to and from organs,
Related tests include:
- Brain PET scan
- Breast PET scan
- Heart PET scan
- Lung PET scan
How the Test is Performed
A PET scan uses a small amount of radioactive material (tracer). The tracer is given through a vein (IV), most often on the inside of your elbow. The tracer travels through your blood and collects in organs and tissues. This helps the radiologist see certain areas of concern more clearly.
You will need to wait nearby as the tracer is absorbed by your body. This takes about 1 hour.
Then, you will lie on a narrow table that slides into a large tunnel-shaped scanner. The PET detects signals from the tracer. A computer changes the signals into 3-D pictures. The images are displayed on a monitor for your doctor to read.
You must lie still during test. Too much movement can blur images and cause errors.
How long the test takes depends on what part of the body is being scanned.
How to Prepare for the Test
You may be asked not to eat anything for 4 – 6 hours before the scan. You will be able to drink water.
Tell your health care provider if:
- You are afraid of close spaces (have claustrophobia). You may be given a medicine to help you feel sleepy and less anxious.
- You are pregnant or think you might be pregnant.
- You have any allergies to injected dye (contrast).
Always tell your health care provider about the medicines you are taking, including those bought without a prescription. Sometimes, medications may interfere with the test results.
How the Test will Feel
You may feel a sharp sting when the needle with the tracer is placed into your vein.
A PET scan causes no pain. The table may be hard or cold, but you can request a blanket or pillow.
An intercom in the room allows you to speak to someone at any time.
There is no recovery time, unless you were given a medicine to relax.
Why the Test is Performed
A PET scan can reveal the size, shape, position, and some function of organs.
This test can be used to:
- Check brain function
- Diagnose cancer, heart problems, and brain disorders
- See how far cancer has spread
- Show areas in which there is poor blood flow to the heart
Several PET scans may be taken over time to check how well you are responding to treatment for cancer or another illness.
Normal Results
A normal result means there were no problems seen in the size, shape, or position of an organ. There are no areas in which the tracer has abnormally collected.
What Abnormal Results Mean
Abnormal results depend on the part of the body being studied. Abnormal results may be due to:
- Change in the size, shape, or position of an organ
- Cancer
- Infection
- Problem with organ function
Risks
The amount of radiation used in a PET scan about the same amount as for most CT scans. Short-lived tracers are used so the radiation is gone from your body in about 2-10 hours.
Tell your doctor before having this test if you are pregnant or breast feeding. Infants and babies developing in the womb are more sensitive to radiation because their organs are still growing.
Rarely, people may have an allergic reaction to the tracer material. Some people have pain, redness, or swelling at the injection site.
Considerations
It is possible to have false results on a PET scan. Blood sugar or insulin levels may affect the test results in people with diabetes.
Most PET scans are now performed along with a CT scan. This combination scan is called a PET/CT.
Electrocardiogram (EKG)
One of the most common cardiac evaluation tools is an electrocardiogram, which is a simple, painless test that records the heart’s electrical activity. An electrocardiogram is called an EKG or ECG or sometimes a 12-lead EKG or 12-lead ECG because the electrical activity of the heart is most often recorded from 12 different places on the body at the same time.
To understand this test, it helps to understand how the heart works. With each heartbeat, an electrical signal spreads from the top of the heart to the bottom. As it travels, the signal causes the heart to contract and pump blood. The process repeats with each new heartbeat. The heart’s electrical signals set the rhythm of the heartbeat.
An EKG shows how fast your heart is beating, whether the rhythm of your heartbeat is steady or irregular, and the strength and timing of electrical signals as they pass through each part of your heart. This test is used to detect and evaluate many heart problems, such as heart attack, arrhythmia, and heart failure. EKG results also can suggest other disorders that affect heart function.
Your doctor may recommend an electrocardiogram (EKG) if you have signs or symptoms that suggest a heart problem. Examples of such signs and symptoms include:
- Chest pain
- Heart pounding, racing, or fluttering, or the sense that your heart is beating unevenly
- Problems breathing
- Feeling tired and weak
- Unusual heart sounds when your doctor listens to your heartbeat
You may have an EKG so your doctor can check how well heart medicine or a medical device, such as a pacemaker, is working. The test also may be used for routine screening before major surgery.
How to prepare for an electrocardiogram
No special preparation is needed for an electrocardiogram (EKG). Before the test, let your doctor know what medicines you’re taking. Some medicines can affect EKG results.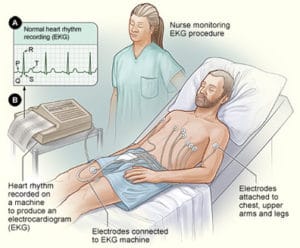
The illustration shows the standard setup for an EKG. In figure A, a normal heart rhythm recording shows the electrical pattern of a regular heartbeat. In figure B, a patient lies in a bed with EKG electrodes attached to his chest, upper arms, and legs. A nurse watches the painless procedure.
What To Expect During an Electrocardiogram?
A technician attaches soft, sticky patches called electrodes to the skin of your chest, arms, and legs. The patches are about the size of a quarter. Typically, 12 patches are attached to detect your heart’s electrical activity from many angles. To help the patches stick, the technician may have to shave areas of your skin. After the patches are placed on your skin, you lie still on a table while the patches detect your heart’s electrical signals. A machine records these signals on graph paper or displays them on a screen. The entire test takes about 10 minutes.
Holter and Event Monitors
Holter and event monitors are medical devices that record the heart’s electrical activity. Doctors most often use these monitors to diagnose arrhythmias. These are problems with the speed or rhythm of the heartbeat. During an arrhythmia, the heart can beat too fast, too slow, or irregularly.
Holter and event monitors also are used to detect silent myocardial ischemia. In this condition, not enough oxygen-rich blood reaches the heart muscle. “Silent” means that no symptoms occur.
These monitors also can check whether treatments for arrhythmia and silent myocardial ischemia are working.
Overview
Holter and event monitors are similar to an EKG (electrocardiogram). An EKG is a simple test that detects and records the heart’s electrical activity. It’s the most common test for diagnosing a heart rhythm problem.
However, a standard EKG only records the heartbeat for a few seconds. It won’t detect heart rhythm problems that don’t occur during the test.
Holter and event monitors are small, portable devices. You can wear one while you do your normal daily activities. This allows the monitor to record your heart for a longer time than an EKG.
Some people have heart rhythm problems that only occur during certain activities, such as sleep or physical exertion. Using a Holter or event monitor increases the chance of recording these problems.
Although similar, Holter and event monitors aren’t the same. A Holter monitor records your heart’s electrical activity the entire time you’re wearing it. An event monitor only records your heart’s electrical activity at certain times while you’re wearing it.
How the Test is Performed
Electrodes (small conducting patches) are stuck onto your chest and attached to a small recording monitor. You carry the Holter monitor in a pocket or small pouch worn around your neck or waist. The monitor is battery operated.
While you wear the monitor, it records your heart’s electrical activity. You should keep a diary of what activities you do while wearing the monitor. After 24 – 48 hours, you return the monitor to your doctor’s office. The doctor will look at the records and see if there have been any irregular heart rhythms.
It is very important that you accurately record your symptoms and activities so that the doctor can match them with your Holter monitor findings.
How to Prepare for the Test
There is no special preparation for the test. Your doctor will start the monitor. You’ll be told how to replace the electrodes should they fall off or become loose.
Tell your doctor if you are allergic to any tape or other adhesives. Make sure you shower or bathe before you start the test. You will not be able to do so while you are wearing a Holter monitor.
How the Test Will Feel
This is a painless test. However, some people may need to have their chest shaved so the electrodes can stick.
You must keep the monitor close to your body. This may make sleeping difficult for some people.
You should continue your normal activities while wearing the monitor.
Why the Test is Performed
Holter monitoring is used to determine how the heart responds to normal activity. The monitor may also be used:
- After a heart attack
- To diagnose heart rhythm problems
- When starting a new heart medicine
It may be used to diagnose:
- Atrial fibrillation/flutter
- Multifocal atrial tachycardia
- Palpitations
- Paroxysmal supraventricular tachycardia
- Reasons for fainting
- Slow heart rate (bradycardia)
- Ventricular tachycardia
Normal Results
Normal variations in heart rate occur with activities. A normal result is no significant changes in heart rhythms or pattern.
What Abnormal Results Mean
Abnormal results may include various arrhythmias. Changes may mean that the heart is not getting enough oxygen.
The monitor may also detect conduction block, a condition in which the atrial electrical activity is either delayed or does not continue into the ventricles of the heart.
Risks
There are no risks associated with the test. However, you should be sure not to let the monitor get wet.

